WE ARE NOW OFFERING COVID-19 (CORONA VIRUS) TESTING.
Receive testing kits within 2-4 days. You can immediately return specimens for testing and results should be to you within 48-72 hours via online portal. Contact us for details.
PCR TESTING OF INFECTIOUS PATHOGENS
CULTURES ARE NON-PRODUCTIVE
We offer PCR (Polymerase Chain Reaction) testing for a number of infectious pathogens including: Upper Respiratory, Sinus (ENT), Urinary Tract (UTI), Vaginitis, Sexually Transmitted Infections (STI), Wound Care, Dermatology, Orthopedic and other skin ailments.
With PCR Testing you are able to know exactly which micro-organisms are present in any given infection. Especially when multiple viral and multiple bacterial pathogens can be found residing within the same infection. PCR allows us to match the bacterial and fungal DNA/RNA from your sample to all the known pathogens within the study spaces listed above. Once the pathogenic organisms are identified, medications can be selected and ratios adjusted to specifically address that individual. Thereby allowing for a precise treatment that ultimately expedites healing - 4 to 6 - times faster without recurring events. These specifically developed treatments are often referred to as Personalized Medicine. Furthermore, most insurance companies cover our services.
Antibiotic Stewardship with ABXASSIST - Get Antibiotic Resistance Results that are more accurate than culture.
Better Diagnostics – Molecular Pathology Detection
Rapid Results – 24 hours after sample arrival at lab
Comprehensive Offering - Ability to detect over 125 pathogens
Resistance Gene Identification (30 resistance genes - largest panel on the commercial market)
Sanford Guide Integration, the most trusted source in the treatment of infectious disease
Antibiotic Spectrum Classification
FDA Guidance Documentation
Antibiotic Cost Data
Easy Access – mobile, web-portal or EHR Integration
INFECTIONS - Upper Respiratory, Sinus (ENT), Wound, Vaginitis, STI, UTI, Ortho, Derm and other Skin ailments.
The dramatic advantages we offer over traditional culture based analysis have been clearly proven through years of PCR studies. The culture and sensitivity test are antiquated and insufficient for the majority of infections. It is well known that multiple micro-organisms can and do grow in any given infection. Culture can typically only grow one organism and their is no guarantee that it is the most prominent or the most dangerous organism within the infection. The following are some of the findings:
99% of all infections are polymicrobial or biofilm, with high abundance levels.
This means that there are almost always many different organisms present in an infection or wound contributing to the infected state. The challenge here is that many of these microorganisms are very different from each other, and require special attention. A culture cannot grow a biofilm or even multiple organisms.
Less than 5% of known infection microbes can be grown using traditional culture techniques.
This means that the majority of the microbes (over 95%) contributing to the community of organisms within the biofilm or infection allowing the infection or wound to persist will NOT be detected using traditional culture techniques. The culture is inaccurate and with it the resulting sensitivity test.
The limitations of traditional culture techniques lead to increased treatment cost through lack of antibiotic stewardship, longer treatment times, more invasive medical interventions, and a higher incidence of progressed complications. Most importantly, this leads to increased pain and suffering.
This diagnostic empowers the physician to treat the bioburden with DNA level certainty. The microbial Bioburden is a significant barrier for all infections, regardless of etiology.
As a universal barrier, we must make it a universal strategy to utilize molecular diagnostics to maximize healing outcomes. The microbial Bioburden is the only barrier to healing completely in the clinician’s control to manage. (Journal of Wound Care 2011; 20: 5, 232)
WE CAN GUARANTEE THAT THERE IS NO MORE ACCURATE METHOD OF TESTING FOR MICROBIAL ANALYSIS THAN MOLECULAR DNA ANALYSIS (PCR).
Bacteria grow as either individual (planktonic) cells or in complex communities of cells called biofilms. Infections caused by biofilms, often harboring many different types of micro-organisms, have been shown to be much more resistant to treatment. It is now believed that over 99 percent of all bacteria live as a community and attach to surfaces as biofilms. According to the National Institutes of Health, it is believed that approximately 80 percent of all infections in humans are related to biofilms. With molecular diagnostics physicians are able to know exactly which pathogenic micro-organisms are present in any biofilm. Biofilms have been shown to play a role in many infections of the ear, nose, throat, and respiratory tract, including: recurrent acute otitis media, otitis media with effusion, cholesteatoma, chronic tonsillitis, chronic pharyngitis, chronic rhinosinusitis, epiglottitis, laryngotracheitis, pneumonia, and infections of tracheostomies, endotracheal tubes, tympanostomy tubes, pulmonary infections in cystic fibrosis, chronic bronchitis and bronchiolitis.
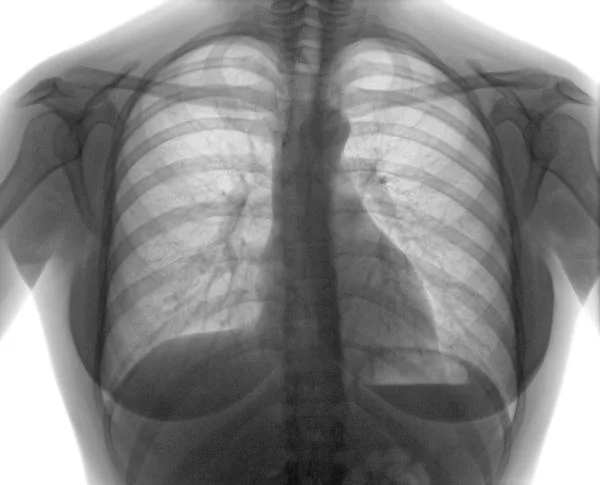
Researchers are estimating that about 200 million people are infected by viral community-acquired pneumonia every year. Approximately 100 million of these cases are children, and 100 million are adults. Molecular diagnostic (PCR) tests have shed light on the role of viruses in pneumonia, and current research indicates that the incidence of viral pneumonia is severely underestimated. In children, dual viral infections are common, and a third of children show evidence of having simultaneous viral and bacterial infections. In adults, viruses are alleged to be the cause of a third of the reported cases of community-acquired pneumonia; in particular influenza viruses, rhinoviruses, and coronaviruses. However, bacteria continue to have a predominant role in adults with pneumonia. Currently, physicians rely on the presence of viral epidemics in the community, a patient's age, speed of illness onset, symptoms, biomarkers, radiographic changes, and response to treatment in order to differentiate viral from bacterial pneumonia. Without molecular diagnostics (PCR), physicians have no clear reason to treat patients with obvious viral community-acquired pneumonia with antibiotics as well. By utilizing both the bacterial and viral molecular diagnostic (PCR) physicians can understand the cause and pathogenesis of community-acquired pneumonia and other respiratory infections, and select the most targeted, effective approach possible to speed patient healing.
EXAMPLE
Say you sent a sample to your normal culture lab and they were able to grow Pseudomonas. They also provided a sensitivity to Pseudomonas which showed that your patients Pseudomonas was resistant to Cipro but sensitive to Levoquin and you prescribe Levoquin.
What value was that when your lab failed to grow the dominant organism in the sample? Fusobacterium is an anaerobe and Levoquin will not touch it. Since you know that for anaerobic bacteria you need to use Clindamycin, Metronidozole, or Augmentin.
DNA sequencing (PCR Testing) will provide the complete picture of all the microbes.